Insulin: A Key Factor in the Nexus of Cardiometabolic Disease
Chief Medical Officer, Metadvice

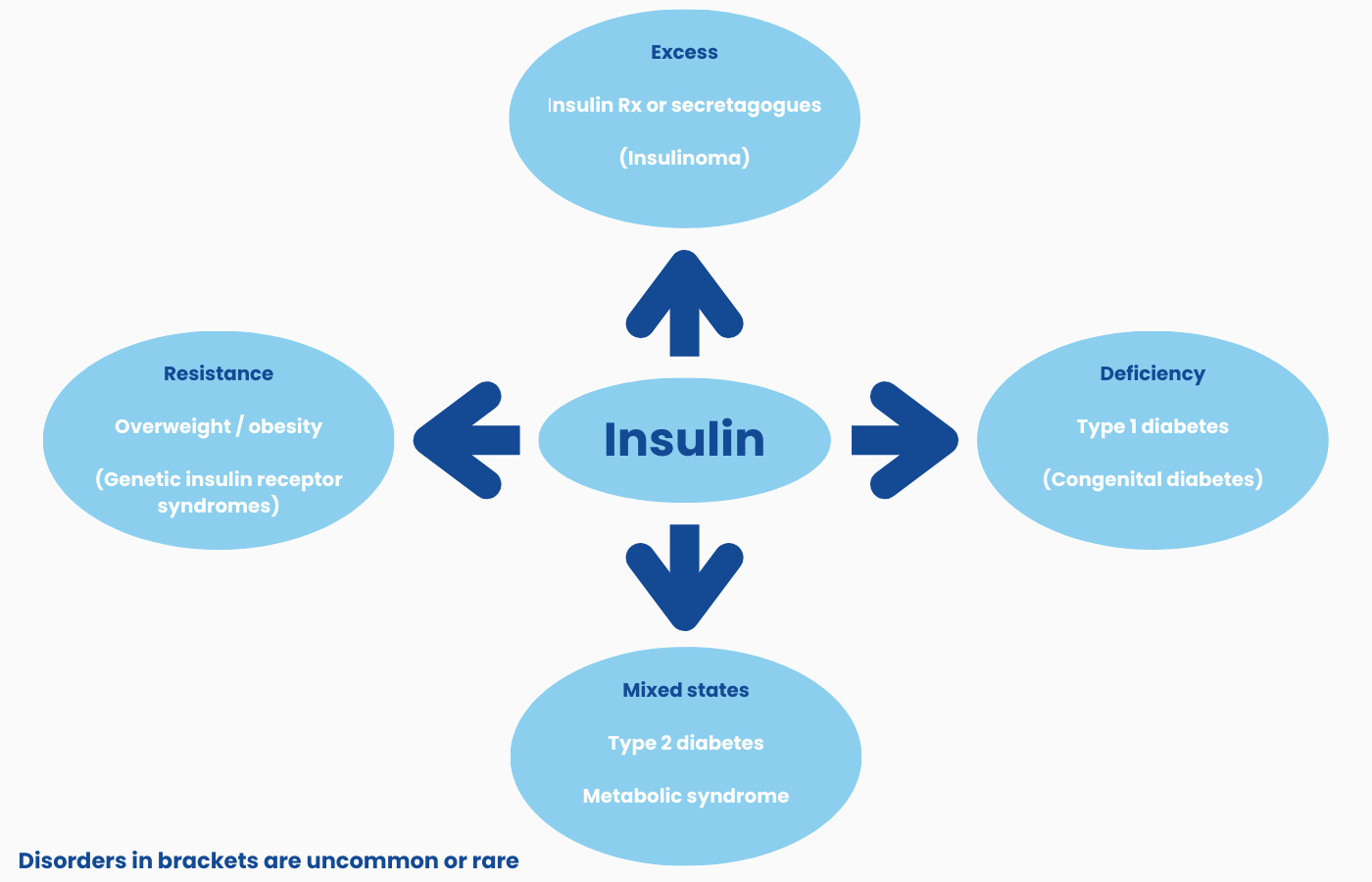
Defects of insulin secretion and/or action are central to the expanding worldwide pandemic of non-communicable cardiometabolic disorders (figure). In recent decades, large scale human overnutrition has fuelled exploding rates of obesity and type 2 diabetes. Uncommon a century ago, type 2 diabetes now affects around 1 in 10 adults worldwide; even greater numbers have degrees of subclinical metabolic dysfunction that predispose to and drive the progression of atherosclerotic cardiovascular disease. Other diseases in which disordered insulin action is considered to play an important role include neurodegenerative disorders (cognitive impairment, dementia), metabolic fatty liver disease, polycystic ovary syndrome, and several types of cancer. Within this complex nexus of closely interwoven disorders, affected individuals often live with a multiplicity of risk factors and progressive cardiometabolic diseases.
NOTES
Degrees of insulin deficiency and insulin resistance often co-exist in mixed states.
Metabolic syndrome denotes a clinical constellation of excess adiposity, glucose intolerance, dyslipidaemia and hypertension. The syndrome overlaps with and contributes to the development and progression of fatty liver disease, renal impairment, polycystic ovary syndrome, and atherosclerosis.
Temporary insulin resistance is a feature of some physiological states, notably the 2nd and 3rd trimesters of pregnancy; the hyperinsulinaemia usually remains subclinical in the absence of concomitant limitations of endogenous insulin secretion.
Insulin deficiency vs insulin resistance
Type 1 diabetes – This is the classic disorder of insulin deficiency. Affected individuals develop a profound insulin deficit requiring life-long replacement therapy. Most often, the cause is selective autoimmune destruction of the insulin-producing ß-cells of the pancreatic islets. The discovery of insulin and its introduction into clinical practice as life-saving therapy for people with type 1 diabetes is one of the most celebrated accomplishments of medical science. Exogenous insulin treatment aims to achieve good metabolic control while avoiding the extremes of hypoglycaemia (resulting from a mismatch of insulin action and insulin requirements1) and hyperglycaemia. However, despite decades of progress and notable technological advances, including the development of insulin analogues, the artificial pancreas, islet and pancreas transplantation, the goal of providing insulin replacement therapy that faithfully approximates normal physiology remains elusive.
Type 2 diabetes – This other major subdivision of diabetes accounts for >90% of all cases. It is closely associated with excess adiposity. The metabolic impact of surplus fat accumulation varies by ethnicity, with non-white populations generally being more adversely affected than white Europeans. While heterogeneity is increasingly recognized, type 2 diabetes usually reflects a combination of relative deficiency of endogenous insulin production in concert with impaired action of the hormone in key metabolically active tissues, i.e., liver, muscle, and adipose tissue. All forms of diabetes – as well as lesser degrees of hyperglycaemia – carry risks of long-term vascular damage. The latter generate an enormous global toll of morbidity and premature mortality. Diabetes-associated small vessel dysfunction damages the eye, kidney, and peripheral nerves. Diabetes also increases the risk of atherosclerotic cardiovascular disease. This necessitates a comprehensive multi-faceted approach to risk reduction that includes careful attention to blood pressure and lipids, in addition to meticulous control of hyperglycaemia. Control of type 2 diabetes often requires insulin therapy to counter waning endogenous production with passing years. Of note, with rising obesity rates, the cluster of cardiovascular risk factors so often associated with type 2 diabetes are now becoming increasingly evident in the context of type 1 diabetes.
Insulin resistance – multiple organs, multiple mechanisms
As well as being a well-documented feature of obesity, type 2 diabetes and metabolic syndrome, insulin resistance is a cardinal biochemical feature of a collection of rare inherited metabolic disorders. As is the case with prevalent acquired forms of insulin resistance, the inherited syndromes are often associated with elevated risks of vascular disease. Informed by these lessons from nature, insulin resistance has come to be recognized as a key biochemical defect in the broader cardiometabolic disease nexus. The biochemical hallmark of insulin resistance is elevated circulating insulin levels accompanied by normo- or hyperglycaemia. Various aspects of insulin action, e.g., insulin-stimulated glucose uptake into muscle, can be assessed using specialised clinical investigative methods such as the hyperinsulinaemic euglycaemic clamp.
Metabolic dysfunction associated steatotic liver disease (MASLD) – The spectrum of disorders associated with defective insulin action has expanded since the earliest descriptions of insulin resistance almost a century ago. MASLD is a prominent example (Read our blog on the subject). This disorder not only confers risks of progressive liver disease and hepatoma, but adds to the burden of atherosclerotic cardiovascular disease in affected individuals. In common with other states of insulin resistance, hepatic steatosis is generally asymptomatic in its early stages.
When communicable disease intersects with non-communicable disease
COVID-19 shone a spotlight on the threats to health associated with cardiometabolic disorders. It rapidly became apparent that affected individuals were at higher risk of severe COVID-related illness and death. As the world started to emerge from the SARS CoV-2 pandemic, it was widely acknowledged that more effective public health efforts were required to improve the health of nations and bolster population-level resilience. However, with some notable exceptions, effective practical public policies aimed at preventing type 2 diabetes remain scarce. The recent news that more than a billion people are now living with obesity2 reinforces the need for redoubling prevention efforts.
The need for a wider clinical perspective of insulin
Advances in precision medicine allied to developments in disease monitoring and an expanding range of therapeutic options require that clinicians and scientists maintain their awareness across the spectrum of diseases in which disordered insulin production and/or action are implicated. Not all require pharmacotherapy. For example, translational research that proceeded from detailed metabolic experiments to large scale clinical trials confirmed the efficacy and safety of low-calorie nutritional interventions. Remission – partial or complete – of type 2 diabetes is possible in many people using this approach, if implemented within the first few years after diagnosis. However, as for GLP-1 receptor agonists, success rates decline with longer-term follow up. Insulin deserves to be better understood by clinicians across a range of medical specialties ranging from primary care physicians (who manage the vast majority of patients with disorders related to insulin) to cardiologists, renal physicians and hepatologists. No longer should consideration of insulin be restricted to the confines of the specialised diabetes clinic.
Metadvice
Metadvice is focused on improving the effectiveness and efficiency of care for people with multiple long-term conditions with an emphasis initially on cardiometabolic disease where disordered insulin physiology is key. Our machine learning technology helps ensure the most appropriate evidence-based interventions at all stages, starting with prevention to the optimal management of late-stage vascular complications. Metadvice is expanding its repertoire of precision medicine tools to address other diseases within the cardiometabolic nexus and then to all long-term chronic conditions.
FOOTNOTES
1 Iatrogenic hypoglycaemia may also be a risk when type 2 diabetes is treated with certain drugs, e.g., sulfonylureas, that stimulate endogenous insulin secretion.
2 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)02750-2/fulltext
3 https://www.directclinicaltrial.org.uk
4 https://drc.bmj.com/content/10/1/e002517
5 Working in the Department of John Macleod at the University of Toronto.
REFERENCE
Krentz AJ (Ed). Insulin: Deficiency, Excess, and Resistance in Human Disease. Academic Press, 2023.
